A Comparative Study of HIER Methods: Online vs Offline Retrieval The objective of this study is to examine the efficiency and effectiveness of heat induced epitope retrieval (HIER) when performed on a fully automated instrument using single-sided application of a heating element and topical dispense of retrieval buffer solution, commonly referred to as online retrieval, […]
Early on, Biocare recognized the market need for evaluating morphologically distinct markers to aid in solving complex clinical problems and simplifying interpretation, all while conserving precious patient tissue. The most glaring clinical need was determined to be the ability to differentiate between prostatic intraepithelial neoplasia (PIN) and carcinoma of the prostate. There also needed to […]
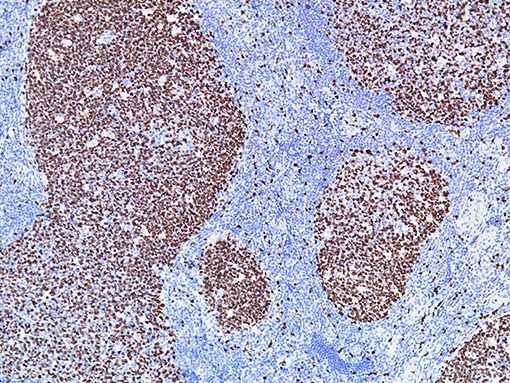
Immunohistochemical staining for programmed cell-death ligand 1 (PD-L1) in malignant thymoma and thymic carcinoma. Alexei Shimanovsky, Richard Cartun, Mary Fiel-Gan, Daniza Mandich, Jonathan Earle, Andrew L. Salner… Abstract e20003 Background: Recent development of anti-PD-1/L1 antibodies has demonstrated activity in various neoplasms. Thymic malignancies (TMS) are rare and treatment in advanced disease is limited. To evaluate […]